Things to know about endometrial ablation procedure

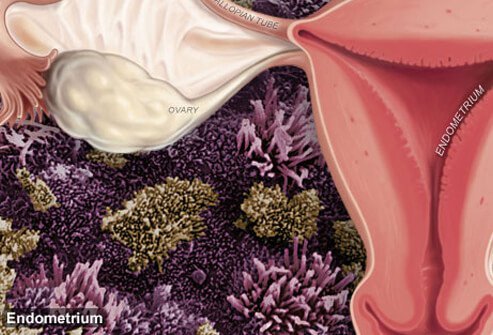
Endometrial ablation is a surgical procedure to remove part of the inner lining of the uterus (endometrium) to cure non-cancerous disorders that cause abnormal uterine bleeding.
- Endometrial ablation is the surgical destruction of the lining tissues of the uterus.
- Endometrial ablation is one type of treatment for abnormal uterine bleeding that is due to a benign (non-cancerous) condition.
- Endometrial ablation must not be performed if pregnancy is desired in the future.
- The laser beam, electricity, freezing, and heating are all successfully used methods for endometrial ablation. The choice of procedure depends upon a number of factors.
- Some women may experience regrowth of the endometrium and require further surgery.
- The majority of patients who had the endometrial ablation procedure report a successful reduction in abnormal bleeding.
What is endometrial ablation?
Endometrial ablation is the surgical destruction of the lining tissues of the uterus, known as the endometrium. Endometrial ablation is one type of treatment for abnormal uterine bleeding.
Why is endometrial ablation done?
Endometrial ablation is a treatment for abnormal bleeding of the uterus that is due to a benign (non-cancerous) condition. Endometrial ablation is not sufficient treatment when the cause of bleeding is cancer of the uterus, since cancer cells may have grown into the deeper tissues of the uterus and cannot often be removed by the procedure.
- Endometrial ablation is only performed on females who are not pregnant and do not plan to become pregnant in the future.
- It should not be performed if the woman has an active infection of the genital tract.
- This treatment is not a first-line therapy for heavy bleeding.
- It should only be considered when medical and hormonal therapies have not been sufficient to control the bleeding.

How is endometrial ablation performed?

To begin the procedure, the cervical opening is dilated to allow passage of the instruments into the uterine cavity.
Prior to the procedure, a woman needs to have an endometrial sampling (biopsy) performed to exclude the presence of cancer. Imaging studies and/or direct visualization with a hysteroscope (a lighted viewing instrument that is inserted to visualize the inside of the uterus) are necessary to exclude the presence of uterine polyps or benign tumors (fibroids) beneath the lining tissues of the uterus. Polyps and fibroids are possible causes of heavy bleeding that can be simply removed without ablation of the entire endometrium. Obviously, the possibility of pregnancy must be excluded, and intrauterine contraceptive devices (IUDs) must be removed prior to endometrial ablation.
Hormonal therapy may be given in the weeks prior to the procedure (particularly in younger women), in order to shrink the endometrium to an extent where ablation therapy has the greatest likelihood of success. The belief is the thinner the endometrium, the greater the chances for successful ablation.
To begin the procedure, the cervical opening is dilated to allow passage of the instruments into the uterine cavity. Different procedures have been used and are all similarly effective for destroying the uterine lining tissue. These include laser beams, electricity, freezing, and heating.
The choice of procedure depends upon a number of factors, including
- the surgeon’s preference and experience,
- the presence of fibroids, the size, and shape of the uterus,
- whether or not pretreatment medication is given, and
- type of anesthesia desired by the patient.
The type of anesthesia required depends upon the method used, and some endometrial ablation procedures can be performed with minimal anesthesia during an office visit. Others may be performed in an outpatient surgery center.
SLIDESHOW
What Is Endometriosis? Symptoms, Causes, Treatment See Slideshow
What are the risks and complications of endometrial ablation?
Complications of the procedure are not common but may include:
- accidental perforation of the uterus,
- tears or damage to the cervical opening (the opening to the uterus), and
- infection, bleeding, and burn injuries to the uterus or intestines.
In very rare cases, the fluid used to expand the uterus during the procedure can be absorbed into the bloodstream, leading to fluid in the lungs (pulmonary edema).
Some women may experience regrowth of the endometrium and need further surgery (see below).
Minor side effects from the procedure can occur for a few days, including cramping (like menstrual cramps), nausea, and frequent urination that may last for 24 hours. A watery discharge mixed with blood may be present for a few weeks after the procedure and can be heavy for the first few days.
What is the outlook after endometrial ablation?
The majority of women who undergo endometrial ablation report a successful reduction in abnormal bleeding. Up to half of the women will stop having periods after the procedure. Yet, studies indicate the rate of failure (defined as bleeding or pain after endometrial ablation that required hysterectomy or reablation) was 16% to 30% at five 5 or years. Failure was most likely to occur in women younger than 45 years and in women with 5 or more children, prior tubal ligation, and a history of painful menstrual cramps. After endometrial ablation, 11% to 36% of women had a repeat ablation or other uterine-sparing procedure.
Although the procedure removes the uterine lining and typically results in infertility, it should not be considered as a birth control measure, because pregnancy can still occur in a small portion of the endometrium that remains or has regrown. In this case, there may be severe problems with the pregnancy, and the procedure should never be performed if the woman may desire pregnancy in the future.
Latest Women’s Health News
Daily Health News
Trending on MedicineNet
Medically Reviewed on 5/25/2022
References
Picket, SD, MD, et al. Endometrial Ablation. Medscape. Updated: Nov 20,2016.