Latest Depression News
 By Cara Murez HealthDay Reporter
By Cara Murez HealthDay Reporter
MONDAY, April 18, 2022 (HealthDay News)
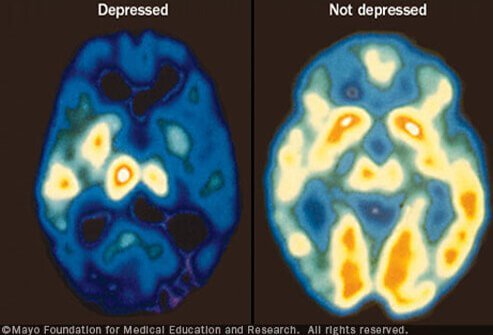
The future of diagnosing and targeting treatments for serious mental health disorders may include MRI brain scans.
Researchers in the United Kingdom found that brain scans enabled them to identify which patients with major depression or psychosis were most likely to have poor outcomes.
That could help doctors decide who might need more intensive treatment from the outset and help them avoid trial-and-error in choosing medications.
While diagnosing conditions like depression, schizophrenia and bipolar disorder is now done by using a patient’s symptoms, medical history and clinical observations, MRI scans would provide biological insights, according to the study.
“We feel that the results of this study can get us a step closer toward using brain scans or other neurobiological information, such as blood samples, for creating more targeted approaches in the treatment of people with psychosis and depression,” said lead author Paris Lalousis, a post-doctoral research fellow at the University of Birmingham, in England.
Though other research has used brain scans for diagnosis and prognosis of mental health, they are not now used clinically, Lalousis said.
For the new study, his team used data from about 300 participants in a European study dubbed PRONIA, which is investigating tools for predicting psychosis. Study participants were diagnosed with recent-onset psychosis or depression.
The researchers sorted them into two groups using a machine learning algorithm. The two groups, or clusters, each contained patients with psychosis and with depression, and each cluster had distinctive characteristics that shed light on patients’ likelihood of recovery.
In the first cluster, lower volumes of gray matter were associated with poorer outcomes.
Gray matter is darker tissue in the brain that is involved in muscle control, memory, emotions and decision-making.
That cluster also had higher levels of inflammation, poorer concentration, and other thinking and memory impairments.
In contrast, higher levels of gray matter in the second cluster signaled that patients were more likely to recover well.
The researchers used a second algorithm to predict patients’ condition nine months after diagnosis, finding this to be more accurate than traditional diagnosis, according to the study.
The team also tested the clusters in other large studies from the United States and Germany, which included individuals who had chronic conditions, not just those newly diagnosed. The longer it had been since diagnosis, the more likely it was that a patient would fall into the cluster with low gray matter, the study found.
“What this tells us is that we have potentially an identifiable signature of poor outcome in early-onset patients,” Lalousis said.
On the other hand, the second cluster showed a potential signature of people who may not need as much intensive treatment, he added.
The researchers now plan to check their results before planning larger clinical trials.
“What we would need to do now is go into the clinic and apply those models and see if people get stratified based on those models compared to just the traditional diagnosis that we have,” Lalousis said. “If we see a difference in the type of outcomes that they achieve, then we can safely say that these models have truly clinical utility.”
Dr. Steven Siegel, chief mental health and wellness officer and psychiatrist at Keck School of Medicine at the University of Southern California in Los Angeles, reviewed the new report.
He said the findings show the potential for technology to help a doctor get a diagnosis and treatment plan that is much better than average.
“Tests like this even the playing field, so that you’re not relying on getting a really good doctor to get an accurate diagnosis and prognosis,” Siegel said. “This would make that accessible to average doctors.”
While technology may help reduce some health care disparities, Siegel said a potential downside is incorporating it too quickly.
But as the process is refined and disseminated, he imagines that instead of a “yes” or “no” diagnosis, imaging would tell doctors how likely a patient is to be in one cluster instead of another.
SLIDESHOW
Learn to Spot Depression: Symptoms, Warning Signs, Medication See Slideshow
“I would hope that it’s just used as a tool to say we have a little bit more data. It makes us a little bit more comfortable,” Siegel said. “We’ve got some more hard evidence, so to speak, to support my clinical judgment that this is a good course for you.”
Diagnosis will always require context, he pointed out.
For someone with a first major depressive episode, for example, there is good evidence the patient will recover and be fine for the rest of their life, Siegel said. It’s important for them to hear that their brain is still fine, they have lots of potential and great therapies to treat them. With psychosis, imaging won’t change the sense of permanence that already exists, he added.
“I think it’s a piece in the path toward us having a better understanding of what changes in people’s brains early in illness,” Siegel said. “And what I’d love to see is the follow-up study, where they look at people two years later after treatment to see whether some of those patterns are gone.”
The findings were published online April 11 in the journal Biological Psychiatry.
More information
The U.S. National Institute of Mental Health has more about studies of serious mental illnesses.
SOURCES: Paris Lalousis, PhD, post-doctoral research fellow, University of Birmingham, U.K.; Steven Siegel, MD, PhD, chief mental health and wellness officer and psychiatrist, Keck School of Medicine, University of Southern California, Los Angeles; Biological Psychiatry, April 11, 2022, online

Copyright © 2021 HealthDay. All rights reserved.
From 
Depression Resources
Featured Centers
Health Solutions From Our Sponsors