Generic Name: boceprevir (discontinued)
Other Names: Victrelis (discontinued)
Drug Class: HCV Protease Inhibitors
What is boceprevir, and what is it used for?
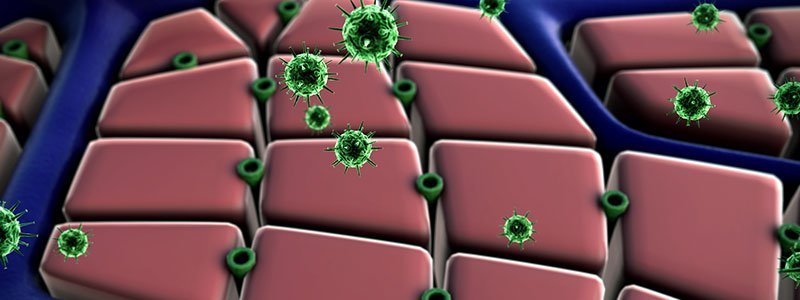
Boceprevir is a man-made antiviral medication that targets hepatitis C virus (HCV). Similar drugs include simeprevir (Olysio) and telaprevir (Incivek).
These drugs are called direct-acting antiviral agents because they act directly on hepatitis C virus. They block the replication of hepatitis C virus in human cells by binding to and inhibiting protease enzymes that HCV use for reproducing. Inhibiting viral replication reduces HCV viral load in the body to undetectable levels in some patients.
The FDA approved boceprevir in March 2011. It was discontinued in 2015.
What are the side effects of boceprevir?
Side effects of boceprevir include
- hair loss,
- dry skin,
- diarrhea,
- loss of appetite,
- nausea,
- altered taste senses,
- sleeplessness,
- irritability,
- fatigue,
- shivering,
- anemia, and
- low white blood cell count.
Boceprevir can cause serious skin reactions, including
- urticaria,
- angioedema,
- Stevens Johnson syndrome (SJS),
- drug reaction with eosinophilia and systemic symptoms (DRESS), and
- exfoliative dermatitis.
Boceprevir should be discontinued if serious skin reactions occur.
What is the dosage for boceprevir?
Dosage Forms and Strengths
Capsule
Dosage Considerations – Should be Given as Follows:
Chronic Hepatitis C
- Discontinued; sale and distribution of boceprevir will be discontinued in the United States by December 2015
- Indicated for the treatment of chronic hepatitis C (CHC) genotype 1 infection in combination with peginterferon alfa and ribavirin
- The indication is specifically for adults with compensated liver disease, including cirrhosis, who are previously untreated or who have failed previous interferon and ribavirin therapy
- Initiate therapy with peginterferon alfa and ribavirin for 4 weeks, THEN
- Add boceprevir 800 mg orally every 8 hours (i.e., every 7-9 hours) with food
Treatment Duration
Duration of treatment depends on HCV-RNA levels at treatment weeks 8, 12, and 24
HCV-RNA levels at 8 weeks
- Previously untreated and HCV-RNA levels undetectable: Complete 3-medication regimen at week 28
- Previously untreated and HCV-RNA levels detectable: Continue 3 medication regimen through week 36, then continue peginterferon alfa and ribavirin through week 48
- Partial responders or relapsed and HCV-RNA levels undetectable: Complete 3-medication regimen at week 36
- Partial responders or relapsed and HCV-RNA levels detectable: Continue 3 medication regimen through week 36, then continue peginterferon alfa and ribavirin through week 48
HCV-RNA levels at 12 weeks
- Response-guided therapy was not studied in individuals who had less than a 2-log10 HCV-RNA decline by treatment week 12 during prior therapy with peginterferon alfa and ribavirin
- If considered for treatment, these patients should receive peginterferon alfa and ribavirin for 4 weeks followed by boceprevir for 44 weeks in combination with peginterferon alfa and ribavirin
- In addition, consideration should be given to treating previously untreated patients who are poorly interferon responsive (as determined at TW 4) with 4 weeks peginterferon alfa and ribavirin followed by boceprevir for 44 weeks in combination with peginterferon alfa and ribavirin to maximize rates of a sustained virologic response
HCV-RNA levels at 24 weeks
- If HCV-RNA levels are undetectable at treatment week 24, continue with the treatment regimen identified at week 8
Treatment futility
- Discontinuation of therapy is recommended in all patients with any of the following circumstances:
- If HCV-RNA levels 1000 IU/mL or greater at week 8, discontinue the 3-medication regimen, OR
- If HCV-RNA levels 100 IU/mL or greater at week 12, discontinue the 3-medication regimen, OR
- If confirmed, detectable HCV-RNA levels at week 24, discontinue 3-medication regimen
Compensated cirrhosis
- Peginterferon alfa and ribavirin for 4 weeks followed by boceprevir for 44 weeks in combination with peginterferon alfa and ribavirin
Renal or Hepatic Impairment
- No dose adjustment for boceprevir is required
- See peginterferon alfa and ribavirin monographs for recommended dose adjustments
Administration
- Must be administered in combination with peginterferon alfa and ribavirin
- Administer with a meal or light snack
Which drugs or supplements interact with boceprevir?
- Boceprevir should not be combined with alfuzosin (Uroxatral), doxazosin (Cardura), sildosin (Rapaflo), tamsulosin (Flomax), sildenafil (Viagra), and tadalafil (Cialis) because it can increase their blood levels, leading to increased side effects from these drugs.
- Boceprevir should not be combined with carbamazepine (Tegretol), phenobarbital, phenytoin (Dilantin), rifampin, and St. John’s wort because they can increase the breakdown of boceprevir and decrease its effectiveness.
- Boceprevir should not be combined with lovastatin (Mevacor) and simvastatin (Zocor) due to increased risk of muscle aches, including rhabdomyolysis.
- Boceprevir should be combined with midazolam (Versed) and triazolam (Halcion) because of increased risk of sedation and respiratory depression.
- Boceprevir should be used with caution with HIV medications like atazanavir (Reyataz), ritonavir, (Norvir), darunavir (Prezista), and lopinavir/ritonavir (Kaletra) because it leads to fluctuating levels of boceprevir and the HIV medications, leading to decreased effectiveness.
- Boceprevir should be used with caution with arrhythmia medications because the combination can increase the risk of irregular heart rate and rhythm.
- Boceprevir should be used with caution with antifungal medications like ketoconazole (Nizoral), itraconazole (Sporanox), and voriconazole (Vfend); antibiotics like clarithromycin (Biaxin) and erythromycin (Erythrocin); immunosuppressant medications like cyclosporine (Gengraf, Neoral, Sandimmune), tacrolimus (Prograf), and sirolimus (Rapamune). Boceprevir can slow the breakdown of these medications and increase their levels in the body, leading to increased side effects and toxicity.
- Boceprevir should be used with caution with warfarin because it can increase or decrease warfarin breakdown, increasing or decreasing the effect of warfarin.
QUESTION
Hepatitis C virus causes an infection of the ______________. See Answer
Is boceprevir safe to take if I’m pregnant or breastfeeding?
- Boceprevir is combined with ribavirin and peginterferon alfa, which cause fetal harm and birth defects if used in pregnant women or in male partners of women who are pregnant.
- Female patients of childbearing potential and their male partners as well as male patients and their female partners must use two effective birth control methods during treatment and for 6 months after treatment.
- Female patients should have monthly pregnancy tests during treatment and for 6 months after stopping treatment.
- It is not known whether boceprevir enters breast milk; therefore, it is best to be cautious before using it in nursing mothers. To avoid any potential risk to the newborn, a decision must be made to discontinue nursing or to discontinue the drug.
What else should I know about boceprevir?
Do I need a prescription for boceprevir?
What preparations of boceprevir are available?
- Capsule, 200 mg
How should I keep boceprevir stored?
- Boceprevir should be refrigerated at 2 C to 8 C (36 F 46 F) until dispensed. Refrigerated boceprevir can remain stable until the expiration date. Boceprevir can also be stored at room temperature up to 25 C (77 F) for 3 months.
- Boceprevir should be stored in tightly closed containers, avoiding exposure to excessive heat.
Latest Digestion News
Daily Health News
Trending on MedicineNet
Medically Reviewed on 6/9/2022
References
FDA Prescribing Information
https://reference.medscape.com/drug/victrelis-boceprevir-999655